Introduction
Each year, more than 8 million children in the U.S. are evaluated in emergency departments (EDs) following blunt trauma, but less than 1% are diagnosed with cervical spine injuries (CSI). Computed tomography (CT) scans are often used to evaluate for CSIs. This exposes children to ionizing radiation increasing their lifetime risk of cancer. A newly published Lancet study, “A Cervical Spine Injury Prediction Rule for Children After Blunt Trauma,” led by Dr. Julie Leonard, was conducted to develop and validate a clinical prediction rule to identify children at risk of CSI after blunt trauma that could minimize unnecessary radiation exposure from CT scan use.
Study question
Can a reliable clinical prediction rule be developed to identify cervical spine injuries (CSIs) in pediatric patients after blunt trauma, minimizing unnecessary radiographic imaging?
Study design
The study enrolled children <18 years who experienced blunt trauma and were evaluated at 18 EDs affiliated with the Pediatric Emergency Care Applied Research Network. Data regarding physical signs and symptoms were collected from the treating ED clinicians. Factors associated with risk for CSI were identified in a multistep process that included logistic and Poisson regression, and classification and regression tree analysis for the final design of the decision rule. The sensitivity, specificity, positive predictive value, and negative predictive value of the rule were assessed with an independent validation cohort.
Results
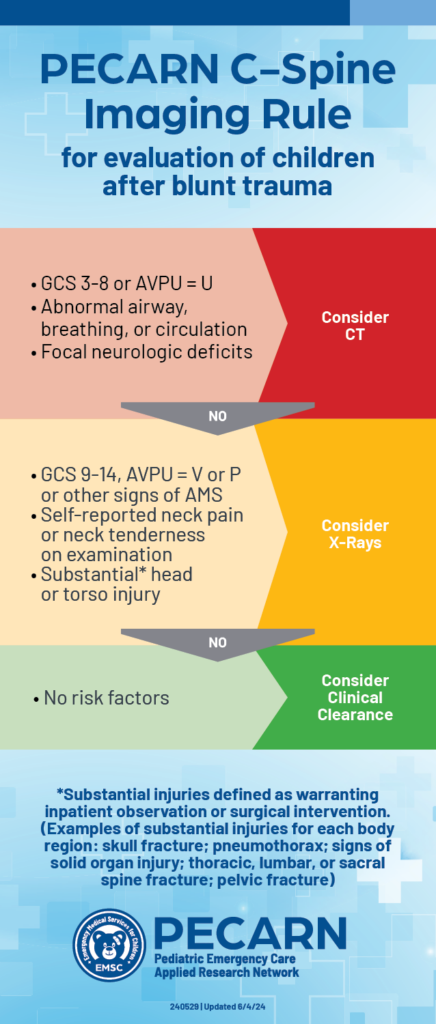
Out of 22,430 children included in the study, 433 (1.9%) were found to have CSI. The study identified 4 high risk factors for CSI to be used to triage children to CT (12% risk for a cervical spine injury):
- Glasgow Coma Scale scores of 3-8
- Unresponsiveness to on the AVPU scale
- Abnormal airway/breathing/circulation
- Focal neurologic deficits
In children without high-risk findings, 5 additional findings identified children with intermediate, non-negligible risk of CSI (3.6% risk of a cervical spine injury):
- Altered mental status
- Substantial head
- Substantial torso injury
- Midline neck pain
- Midline neck tenderness
Notably this risk stratification approach towards identifying high and intermediate risk traumatic injuries mirrors the PECARN clinical decision tool for blunt head trauma. In our study, high risk findings generally warrant CT imaging and intermediate risk findings in the absence of high risk findings can start with x-ray imaging. Without any of these risk factors, the patient’s cervical spine can be clinically cleared with any imaging because the risk for a cervical injury is extremely low (0.2%).
Using the risk factors in an imaging algorithm could significantly reduce the use of CT without increasing the use of x-rays. The PECARN CSI prediction rule is clinically sensible and easy to implement in emergency settings.
Figuring out which children need cervical spine imaging after blunt trauma can be a real challenge for even the most seasoned EMS and ED clinicians. We often end up extrapolating rules derived mainly in adults or using pediatric rules based on small retrospective analyses. Thanks to Dr. Leonard’s work, we now have a validated clinical prediction rule based on a large prospective pediatric study. It is exciting that this prediction rule, when used in clinical algorithms, could reduce the number of children receiving unnecessary radiographic testing and radiation exposure.
Caleb Ward, MB BChir, MPH (he/him/his), co-author
Assistant Professor of Pediatrics and Emergency Medicine, The George Washington University School of Medicine and Health Sciences; Associate Research Director, Division of Emergency Medicine, Children’s National Medical Center
Take home messages |
|---|
|
Why is this important for patients and caregivers
A clinical tool can be used by clinicians to minimize unnecessary CT scans and x-rays often used to evaluate for cervical spine (neck) injuries, significantly reducing children’s exposure to harmful ionizing radiation.
The tool is based on specific risk factors for cervical spine injuries, including altered mental status, abnormal airway, breathing or circulation, posterior midline neck pain or tenderness, severe head or torso injuries, and neurologic deficits. This helps emergency department clinicians make more informed decisions about when neck imaging (CT or x-ray) is truly necessary.
This research sets the stage for broader adoption of safer imaging practices in the assessment of injured children, enhancing child safety nationwide.